Life with Being Independent on Insulin is the reality that millions of Americans face. This can be challenging at times. USA Script Helpers gives its readers insight on the following:
- What is Natural Insulin?
After an individual has consumed food, the digestive system works to distribute carbohydrates into the glucose which then makes its way into a person’s bloodstream. An individual who is diabetes free has the pancreas working by producing the required insulin hormone which distributes glucose to an individual’s cells. By doing this, this creates energy. The purpose of insulin is to ensure that glucose levels in a person’s blood are functioning within a narrow range.
- What Is insulin-dependent Diabetes?
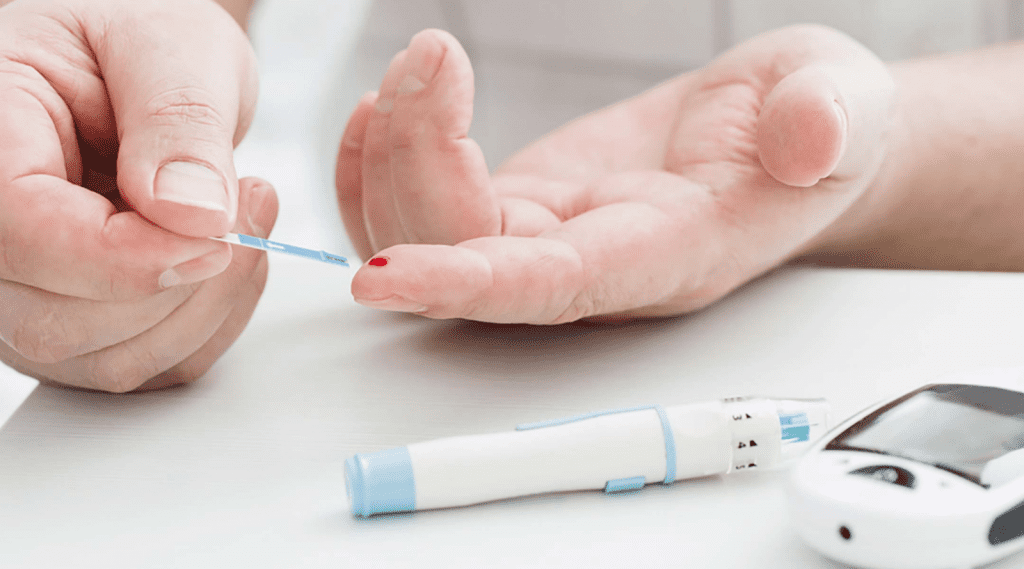
Did you know that if the human body has trouble producing natural insulin (typically this occurs in diabetics living with type 1 diabetes) that both type 1 and type 2 diabetics should always monitor their glucose levels? Glucose levels can increase when an individual consumes food due to the fact that there is not an efficient amount of insulin that helps to circulate the glucose in the body’s cells. Elevated Glucose that is found in the blood can actually create complications that may occur in the following:
- Heart
- Nerves
- Kidneys
- Eyes
To name a few. Be sure to monitor your glucose levels and speak to your doctor or one of our licensed pharmacists from our contracted* pharmacy department. At this day and age there is currently no cure to Diabetes. Therefore, diabetics must monitor and control the glucose found in their blood for a doctor to determine sufficient insulin doses to help the diabetic manage their diabetes.
- What Does Insulin Therapy Do for diabetics living with diabetes?
The purpose of having insulin managed by medications is to control the glucose found in an individual’s blood to help prevent complications to those living as Type 1 diabetics and those living with Type 2 diabetes. Type 2 diabetes requires insulin when tablet medications are no longer able to manage this illness.
- Diabetes – How common is living with diabetes in the USA?
Did you know that over 30 million people of all ages are living in the USA with a form of diabetes? Every year this number significantly increases. There are millions of people who have early stages of diabetes without knowing they have diabetes.
- Diabetes – What are the risk factors?
Type 1 diabetes.. This is when a person’s immune system is working against itself. Risk factors include:
- Any age group
- Family History
Type 2 diabetes. This happens when the body is having problems regulating the blood sugar as a source of fuel. This occurs as a long term condition. It is important to acknowledge that high blood sugar levels have the potential of leading to problems that may attack a person’s immune system.
- Diabetes. What are the symptoms?
Signs of Diabetes may include the following:
- Hunger
- Thirst
- An explained weight loss
- Constant Urination
- Blurred vision
- Numbness or tingle sensation of hands/feet
- Fatigue
- Dizziness
- Short Temper
- Wounds recovering slowly
- Infections
Type 1 Diabetics live with a condition that has no cure. This occurs genetically. Symptoms can develop over a series of time. Type 1 diabetes is when blood sugar levels increase to high levels.
Type 2 diabetics may have the same as above but show less to no symptoms at all.
It is important to acknowledge that although Type 2 diabetes is a less progressed version of type 1 diabetes type 2 diabetics need to be aware that health problems can occur at any time. Studies show that type 2 diabetics live with increased chances of developing heart disease and sometimes stroke.
- How is diabetes detected and diagnosed?
Your doctor can detect diabetes through a blood test. Speak to your doctor or one of our Pharmacists from our contracted* Pharmacy department regarding any questions or concerns you may have regarding both type 1 and type 2 diabetes. Be sure to inform your doctor if you are taking any medications that may affect your blood sugar levels. Or if you have any allergic reaction to anything related to diabetic medications such as tablet and insulin forms.
- What do Diabetics use to help maintain their diabetes?
Those living with diabetes live by using insulin or tablet form medications. There are various insulins available in the market that either work as faster or slower release insulin. Individuals with mild cases of diabetes will use tablet medications or no medications at all to start with when dealing with their illness. To those who have early stages of diabetes, a combination of exercise and a healthy diet might be able to change the course of their futures.
Type of Insulins that Diabetics take are the following:
- Long lasting insulins which would be known as Lantus solostar pens, Lantus Vials, Lantus Cartridge, Basaglar or Toujeo pens, Tresiba pens, Humulin or Novolog pens.
- Short acting/rapid release pens would be known as Novlog or Fiasap Pens. Apidra, Lispro would be Humalog or Admelog or Humulin R or Novloin R pens.
Be sure to speak to your doctor regarding any of the medications that you might need to maintain your illness.
USA Script Helpers is an established Pharmacy Partner with over 10 + years of experience in the online pharmaceutical industry. USA Script Helpers itself is not an online pharmacy but is a pharmacy partner. USA Script Helpers along with it’s contracted* Pharmacy Department offers Americans Customer Support 365 days a year. Check out our website or give us a call at 1 (888) 646-7749 to speak to a member of our team on how to place an order for your medication.